Efficacy and safety demonstrated in the ZUMA-5 pivotal trial
ZUMA-5 study design1,2
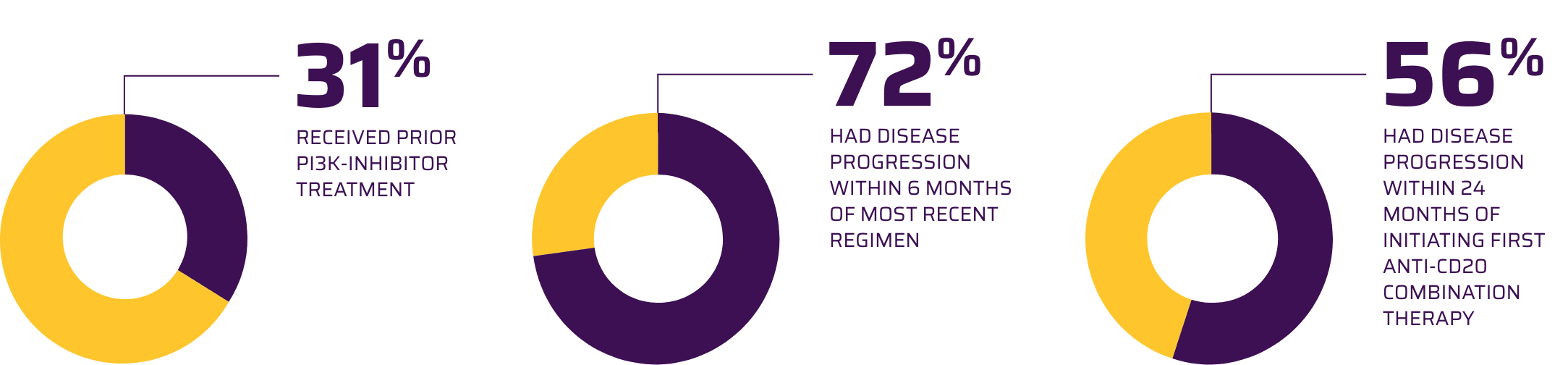
- A phase 2, multicenter, single-arm, open-label study evaluating the efficacy and safety of YESCARTA in adults with R/R FL after ≥2 lines of therapy
- According to the Prescribing Information, 146 patients received YESCARTA and were evaluated for safety
- 81 patients with FL were evaluated for efficacy
- Patients received lymphodepleting chemotherapy: 500 mg/m2 intravenous (IV) cyclophosphamide and 30 mg/m2 IV fludarabine (5, 4, and 3 days before infusion)
- YESCARTA was administered as a single infusion to a target dose of 2 x 106 viable CAR T cells/kg body weight
Primary endpoint: ORR (CR + PR)
Median age: 62 years (range: 34 to 79 years)
Exclusion criteria: Active or serious infections, transformed lymphoma or other aggressive lymphomas, prior allogeneic HSCT, or any history of CNS lymphoma or CNS disorders
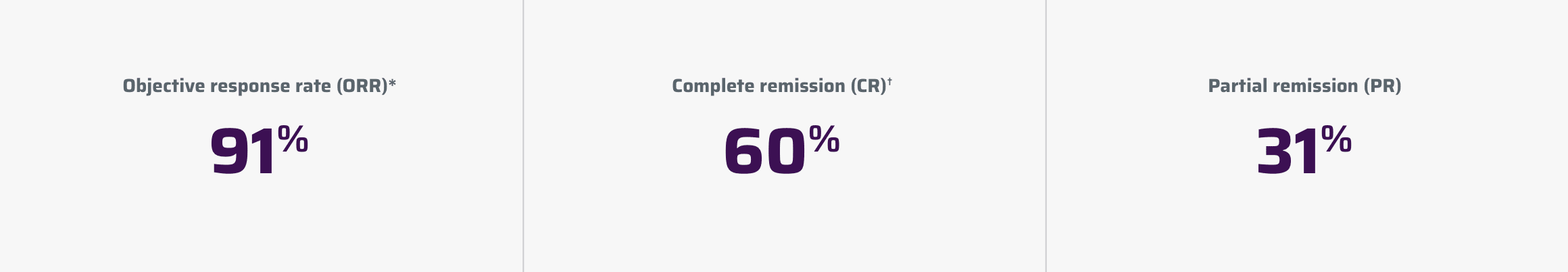
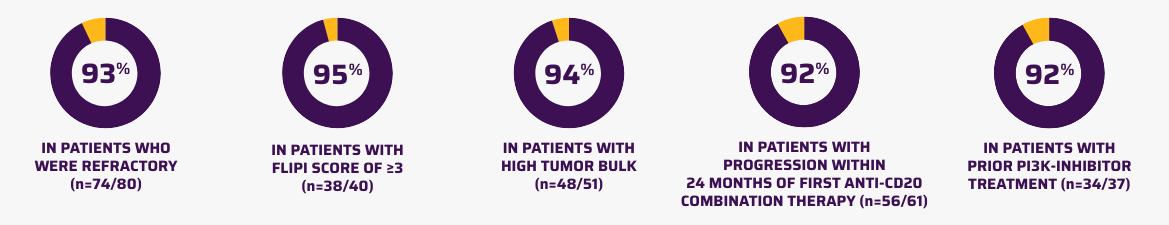
91% of patients with R/R FL responded to YESCARTA1
Pivotal efficacy analysis
*Per the International Working Group Lugano classification (Cheson 2014), as assessed by the independent review committee.1
†Complete remission required documentation of a negative bone marrow biopsy after treatment in patients who did not have a negative bone marrow biopsy between their most recent disease progression prior to ZUMA-5 and initiation of lymphodepleting chemotherapy.1
~36-month follow-up
The ZUMA-5 ~36-month follow-up data were evaluated based on investigator assessment and included 127 patients with FL enrolled in the trial.4 Three of these patients did not receive YESCARTA.1,2 The primary efficacy analysis included in the YESCARTA Prescribing Information was performed using the inferential analysis set, which includes the first 81 of 120 patients enrolled with at least 9 months of follow-up from the date of first response.1,3 For FDA approval, efficacy was evaluated on the basis of ORR and DOR as determined by an IRC.1
Study limitations: These results represent a separate, preplanned, post hoc analysis of the ZUMA-5 study. Data from the ~3-year analysis are descriptive and the follow-up study was not powered or adjusted for multiplicity to assess efficacy. These data are not included in the Prescribing Information for YESCARTA and should be carefully interpreted.
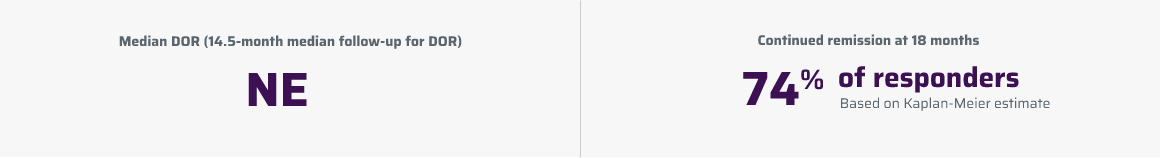
~36-month follow-up: DOR5
DOR was a secondary endpoint of the phase 2, single-arm, open-label ZUMA-5 study.1,2 DOR data are descriptive and should be carefully interpreted in light of the single-arm design. ORR (CR + PR) at 36 months was 94% (119/127).4 In the YESCARTA Prescribing Information, mDOR (n=74 responders) was not estimable at a 14.5-month median follow-up for DOR. The rate of continued remission at 18 months was 74%.1
DOR is measured from the date of first objective response to the date of progression or death from any cause.1
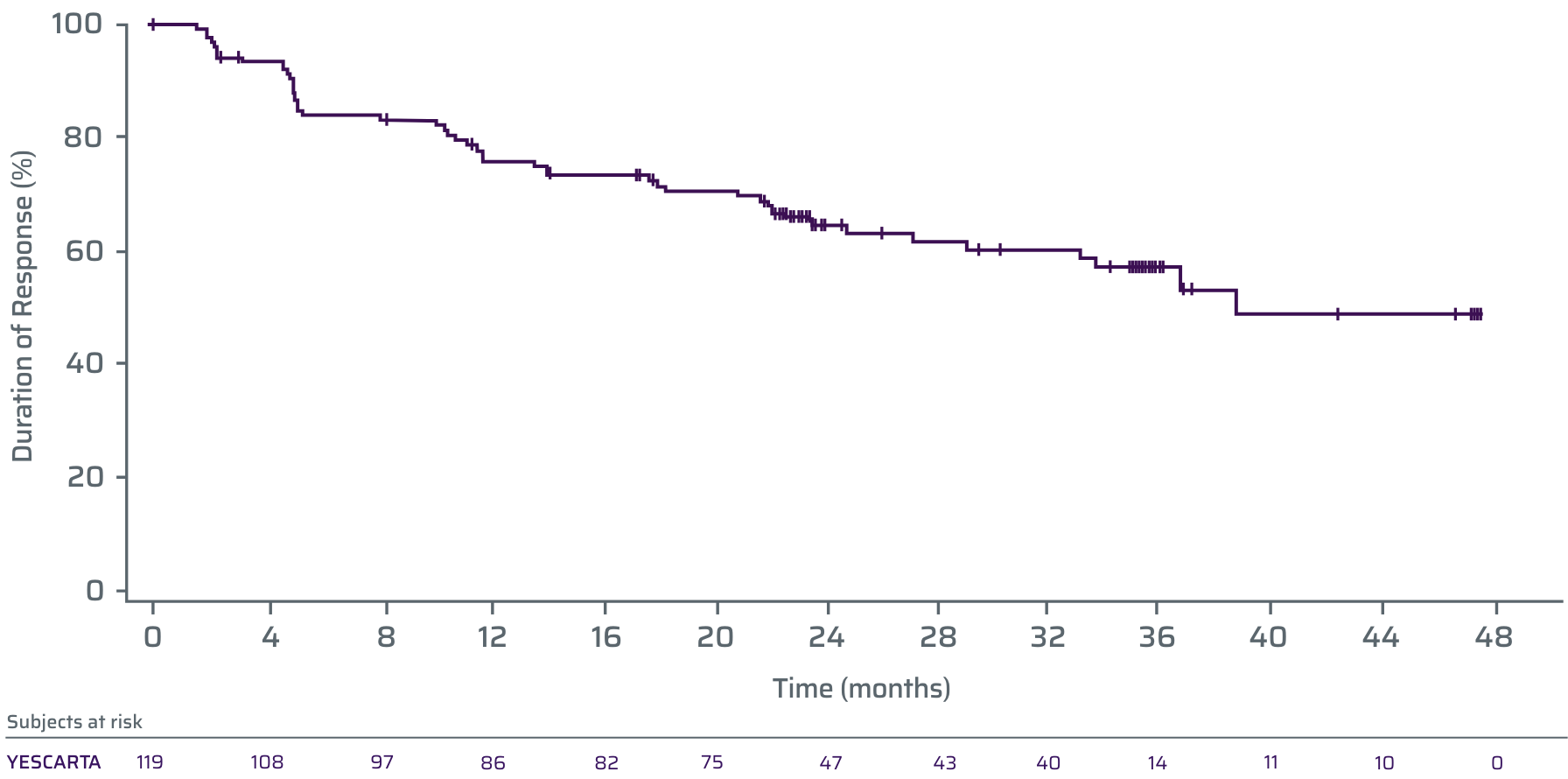
The tick marks represent censored patients. Patients who did not progress, have not died, or received new anti-cancer therapy (including stem cell transplant) prior to documented progression were censored at their last evaluable disease assessment.3
- At a median follow-up of 41.7 months, mDOR was 38.6 months (number of responders=119)4‡
‡KM estimate.5
~36-month follow-up: PFS4
PFS was a secondary endpoint of the phase 2, single-arm, open-label ZUMA-5 study.1,2 PFS data are descriptive and should be carefully interpreted in light of the single-arm design. PFS data are not included in the YESCARTA Prescribing Information.
PFS is based on Kaplan-Meier estimates defined as the time from leukapheresis to date of disease progression or death from any cause.3,4

The tick marks represent censored patients. Patients who did not progress, have not died, or received new anti-cancer therapy (including stem cell transplant) prior to documented progression were censored at their last evaluable disease assessment.3
PFS rate at 36 months was 54% (n=127; 95% CI, 44-64)4
~36-month follow-up: OS4
OS was a secondary endpoint of the phase 2, single-arm, open-label ZUMA-5 study.1,2 OS data are descriptive and should be carefully interpreted in light of the single-arm design. OS data are not included in the YESCARTA Prescribing Information.
OS is defined as the time from the date of leukapheresis to the date of death from any cause.3
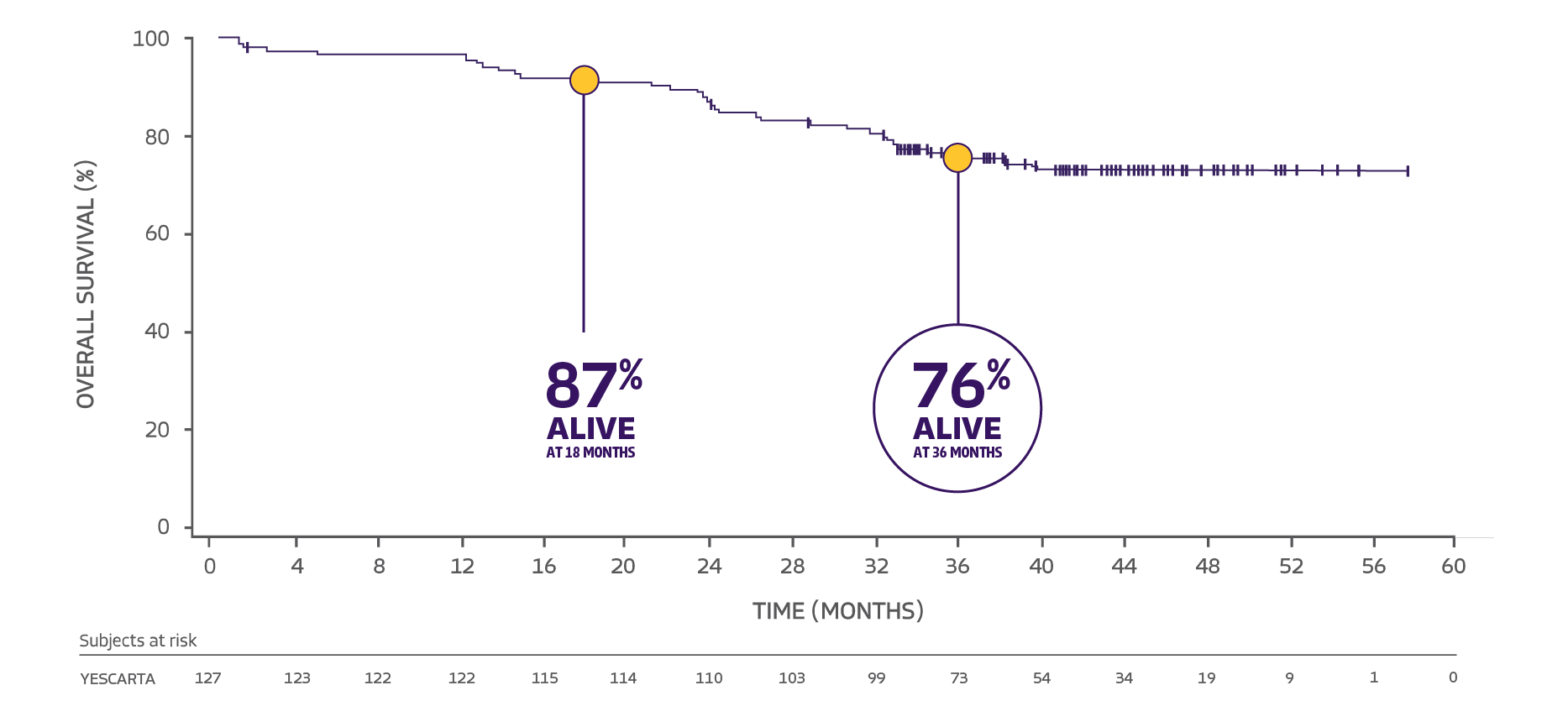
The tick marks represent censored patients. Patients who have not died by the data cutoff date were censored at the last date known to be alive.3
At a median follow-up of 41.7 months, mOS was not estimable4**
**KM estimate.2
CAR=chimeric antigen receptor; CD20=cluster of differentiation; CI=confidence interval; CNS=central nervous system; DOR=duration of response; FDA=Food and Drug Administration; FL=follicular lymphoma; FLIPI=Follicular Lymphoma International Prognostic Index; HSCT=hematopoietic stem cell transplant; iNHL=indolent non-Hodgkin lymphoma; IRC=independent review committee; KM=Kaplan-Meier; mDOR=median duration of response; mOS=median overall survival; mPFS=median progression-free survival; MZL=marginal zone lymphoma; NE=not estimable; NR=not reached; OS=overall survival; PI3K=phosphoinositide 3-kinase; PFS=progression-free survival; R/R=relapsed/refractory.
IMPORTANT SAFETY INFORMATION
WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC TOXICITIES, and SECONDARY HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS), including fatal or life-threatening reactions, occurred in patients receiving YESCARTA. Do not administer YESCARTA to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids.
- Neurologic toxicities, including fatal or life-threatening reactions, occurred in patients receiving YESCARTA, including concurrently with CRS or after CRS resolution. Monitor for neurologic toxicities after treatment with YESCARTA. Provide supportive care and/or corticosteroids as needed.
- T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies, including YESCARTA.
CYTOKINE RELEASE SYNDROME (CRS) CRS, including fatal or life-threatening reactions, occurred following treatment with YESCARTA. CRS occurred in 90% (379/422) of patients with non-Hodgkin lymphoma (NHL), including ≥ Grade 3 CRS in 9%. CRS occurred in 93% (256/276) of patients with large B-cell lymphoma (LBCL), including ≥ Grade 3 in 9%. Among patients with LBCL who died after receiving YESCARTA, 4 had ongoing CRS events at the time of death. For patients with LBCL in ZUMA-1, the median time to onset of CRS was 2 days following infusion (range: 1-12 days) and the median duration was 7 days (range: 2-58 days). For patients with LBCL in ZUMA-7, the median time to onset of CRS was 3 days following infusion (range: 1-10 days) and the median duration was 7 days (range: 2-43 days).
CRS occurred in 84% (123/146) of patients with indolent non-Hodgkin lymphoma (iNHL) in ZUMA-5, including ≥ Grade 3 CRS in 8%. Among patients with iNHL who died after receiving YESCARTA, 1 patient had an ongoing CRS event at the time of death. The median time to onset of CRS was 4 days (range: 1-20 days) and median duration was 6 days (range: 1-27 days) for patients with iNHL.
Key manifestations of CRS (≥ 10%) in all patients combined included fever (85%), hypotension (40%), tachycardia (32%), chills (22%), hypoxia (20%), headache (15%), and fatigue (12%). Serious events that may be associated with CRS include, cardiac arrhythmias (including atrial fibrillation and ventricular tachycardia), renal insufficiency, cardiac failure, respiratory failure, cardiac arrest, capillary leak syndrome, multi-organ failure, and hemophagocytic lymphohistiocytosis/macrophage activation syndrome (HLH/MAS).
The impact of tocilizumab and/or corticosteroids on the incidence and severity of CRS was assessed in 2 subsequent cohorts of LBCL patients in ZUMA-1. Among patients who received tocilizumab and/or corticosteroids for ongoing Grade 1 events, CRS occurred in 93% (38/41), including 2% (1/41) with Grade 3 CRS; no patients experienced a Grade 4 or 5 event. The median time to onset of CRS was 2 days (range: 1-8 days) and the median duration of CRS was 7 days (range: 2-16 days). Prophylactic treatment with corticosteroids was administered to a cohort of 39 patients for 3 days beginning on the day of infusion of YESCARTA. Thirty-one of the 39 patients (79%) developed CRS and were managed with tocilizumab and/or therapeutic doses of corticosteroids with no patients developing ≥ Grade 3 CRS. The median time to onset of CRS was 5 days (range: 1-15 days) and the median duration of CRS was 4 days (range: 1-10 days). Although there is no known mechanistic explanation, consider the risk and benefits of prophylactic corticosteroids in the context of pre-existing comorbidities for the individual patient and the potential for the risk of Grade 4 and prolonged neurologic toxicities.
Confirm that 2 doses of tocilizumab are available prior to infusion of YESCARTA. Monitor patients at least daily for 7 days following infusion for signs and symptoms of CRS. Monitor patients for signs or symptoms of CRS for 2 weeks after infusion. Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time. At the first sign of CRS, institute treatment with supportive care, tocilizumab, or tocilizumab and corticosteroids as indicated.
NEUROLOGIC TOXICITIES Neurologic toxicities including immune effector cell-associated neurotoxicity syndrome (ICANS) that were fatal or life-threatening occurred following treatment with YESCARTA. Neurologic toxicities occurred in 78% (330/422) of patients with NHL receiving YESCARTA, including ≥ Grade 3 in 25%.
Neurologic toxicities occurred in 87% (94/108) of patients with LBCL in ZUMA-1, including ≥ Grade 3 in 31% and in 74% (124/168) of patients in ZUMA-7 including ≥ Grade 3 in 25%. The median time to onset was 4 days (range: 1-43 days) and the median duration was 17 days for patients with LBCL in ZUMA-1. The median time to onset for neurologic toxicity was 5 days (range: 1-133 days) and median duration was 15 days in patients with LBCL in ZUMA-7. Neurologic toxicities occurred in 77% (112/146) of patients with iNHL, including ≥ Grade 3 in 21%. The median time to onset was 6 days (range: 1-79 days) and the median duration was 16 days. Ninety-eight percent of all neurologic toxicities in patients with LBCL and 99% of all neurologic toxicities in patients with iNHL occurred within the first 8 weeks of YESCARTA infusion. Neurologic toxicities occurred within the first 7 days of infusion in 87% of affected patients with LBCL and 74% of affected patients with iNHL.
The most common neurologic toxicities (≥ 10%) in all patients combined included encephalopathy (50%), headache (43%), tremor (29%), dizziness (21%), aphasia (17%), delirium (15%), and insomnia (10%). Prolonged encephalopathy lasting up to 173 days was noted. Serious events, including aphasia, leukoencephalopathy, dysarthria, lethargy, and seizures occurred. Fatal and serious cases of cerebral edema and encephalopathy, including late-onset encephalopathy, have occurred.
The impact of tocilizumab and/or corticosteroids on the incidence and severity of neurologic toxicities was assessed in 2 subsequent cohorts of LBCL patients in ZUMA-1. Among patients who received corticosteroids at the onset of Grade 1 toxicities, neurologic toxicities occurred in 78% (32/41) and 20% (8/41) had Grade 3 neurologic toxicities; no patients experienced a Grade 4 or 5 event. The median time to onset of neurologic toxicities was 6 days (range: 1-93 days) with a median duration of 8 days (range: 1-144 days). Prophylactic treatment with corticosteroids was administered to a cohort of 39 patients for 3 days beginning on the day of infusion of YESCARTA. Of those patients, 85% (33/39) developed neurologic toxicities; 8% (3/39) developed Grade 3 and 5% (2/39) developed Grade 4 neurologic toxicities. The median time to onset of neurologic toxicities was 6 days (range: 1-274 days) with a median duration of 12 days (range: 1-107 days). Prophylactic corticosteroids for management of CRS and neurologic toxicities may result in higher grade of neurologic toxicities or prolongation of neurologic toxicities, delay the onset, and decrease the duration of CRS.
Monitor patients for signs and symptoms of neurologic toxicities following infusion at least daily for 7 days; and for 2 weeks thereafter and treat promptly. Advise patients to avoid driving for at least 2 weeks following infusion.
HYPERSENSITIVITY REACTIONS Allergic reactions may occur with the infusion of YESCARTA. Serious hypersensitivity reactions, including anaphylaxis, may be due to dimethyl sulfoxide (DMSO) or residual gentamicin in YESCARTA.
SERIOUS INFECTIONS Severe or life-threatening infections occurred after YESCARTA infusion. Infections (all grades) occurred in 45% of patients with NHL. Grade 3 or higher infections occurred in 17% of patients, including ≥ Grade 3 infections with an unspecified pathogen in 12%, bacterial infections in 5%, viral infections in 3%, and fungal infections in 1%. YESCARTA should not be administered to patients with clinically significant active systemic infections. Monitor patients for signs and symptoms of infection before and after infusion and treat appropriately. Administer prophylactic antimicrobials according to local guidelines.
Febrile neutropenia was observed in 36% of patients with NHL and may be concurrent with CRS. In the event of febrile neutropenia, evaluate for infection and manage with broad-spectrum antibiotics, fluids, and other supportive care as medically indicated.
In immunosuppressed patients, including those who have received YESCARTA, life-threatening and fatal opportunistic infections including disseminated fungal infections (e.g., candida sepsis and aspergillus infections) and viral reactivation (e.g., human herpes virus-6 [HHV-6] encephalitis and JC virus progressive multifocal leukoencephalopathy [PML]) have been reported. The possibility of HHV-6 encephalitis and PML should be considered in immunosuppressed patients with neurologic events and appropriate diagnostic evaluations should be performed.
Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, has occurred in patients treated with drugs directed against B cells, including YESCARTA. Perform screening for HBV, HCV, and HIV and management in accordance with clinical guidelines before collection of cells for manufacturing.
PROLONGED CYTOPENIAS Patients may exhibit cytopenias for several weeks following lymphodepleting chemotherapy and YESCARTA infusion. Grade 3 or higher cytopenias not resolved by Day 30 following YESCARTA infusion occurred in 39% of all patients with NHL and included neutropenia (33%), thrombocytopenia (13%), and anemia (8%). Monitor blood counts after infusion.
HYPOGAMMAGLOBULINEMIA B-cell aplasia and hypogammaglobulinemia can occur in patients receiving YESCARTA. Hypogammaglobulinemia was reported as an adverse reaction in 14% of all patients with NHL. Monitor immunoglobulin levels after treatment and manage using infection precautions, antibiotic prophylaxis, and immunoglobulin replacement.
The safety of immunization with live viral vaccines during or following YESCARTA treatment has not been studied. Vaccination with live virus vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during YESCARTA treatment, and until immune recovery following treatment.
SECONDARY MALIGNANCIES Patients treated with YESCARTA may develop secondary malignancies. T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies, including YESCARTA. Mature T cell malignancies, including CAR-positive tumors, may present as soon as weeks following infusion, and may include fatal outcomes.
Monitor life-long for secondary malignancies. In the event that a secondary malignancy occurs, contact Kite at 1-844-454-KITE (5483) to obtain instructions on patient samples to collect for testing.
ADVERSE REACTIONS The most common non-laboratory adverse reactions (incidence ≥ 20%) in patients with iNHL in ZUMA-5 included fever, CRS, hypotension, encephalopathy, fatigue, headache, infections with pathogen unspecified, tachycardia, febrile neutropenia, musculoskeletal pain, nausea, tremor, chills, diarrhea, constipation, decreased appetite, cough, vomiting, hypoxia, arrhythmia, and dizziness.
INDICATIONMORE
YESCARTA® is a CD19-directed genetically modified autologous T cell immunotherapy indicated for the treatment of adult patients with relapsed or refractory follicular lymphoma (FL) after two or more lines of systemic therapy.
This indication is approved under accelerated approval based on response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trial(s).
Please see accompanying full Prescribing Information, including BOXED WARNING and Medication Guide.
Authorized Treatment Centers are independent facilities that dispense Kite CAR T therapies. Choice of an Authorized Treatment Center is within the sole discretion of the physician and patient. Kite does not endorse any individual treatment sites.
References: 1. YESCARTA® (axicabtagene ciloleucel). Prescribing information. Kite Pharma, Inc; 2025. 2. Jacobson CA, Chavez JC, Sehgal AR, et al. Axicabtagene ciloleucel in relapsed or refractory indolent non-Hodgkin lymphoma (ZUMA-5): a single-arm, multicentre, phase 2 trial. Lancet Oncol. 2022;23(1):91-103. 3. Jacobson CA, Chavez JC, Sehgal AR, et al. Axicabtagene ciloleucel in relapsed or refractory indolent non-Hodgkin lymphoma (ZUMA-5): a single-arm, multicentre, phase 2 trial. Lancet Oncol. 2022;23(1):91-103 (suppl). doi:10.1016/S1470-2045(21)00591-X 4. Neelapu SS, Chavez JC, Sehgal AR, et al. Three-year follow-up analysis of axicabtagene ciloleucel in relapsed/refractory indolent non-Hodgkin lymphoma (ZUMA-5). Blood. 2024;143(6):496-506. 5. Neelapu SS, Chavez JC, Sehgal AR, et al. Three-year follow-up analysis of axicabtagene ciloleucel in relapsed/refractory indolent non-Hodgkin lymphoma (ZUMA-5). Blood. 2024;143(6):496-506 (suppl). doi:10.1182/blood.2023021243